Antibiotics
About antibiotic treatments
Antibiotics are medicines used to treat bacterial infections. Antibiotics either kill a specific type (or types) of bacteria, or stop them from reproducing and spreading. Antibiotics have been around since the 1920s. Prior to that, people would often die from bacterial infections, for which there were no effective treatments.
Once the power of antibiotic treatments became clear, they were used extensively for decades without realising the consequences of overuse and misuse. This included being used to treat illnesses that patients would have been able to overcome by themselves. They have even been prescribed for conditions that cannot be helped with antibiotics. Sir Alexander Fleming, the discoverer of penicillin, had already warned as long ago as 1936 that misuse of penicillin could give rise to resistance.
A bacterial population can double in size approximately every 20 minutes. They can produce large populations in a very short time. According to Darwin’s theory of natural selection and survival of the fittest, bacteria can become resistant to antibiotics in a very short space of time. As a consequence they are able to evade being killed by antibiotics very quickly. Consequently many of the antibiotic treatments we rely upon are ineffective. People are once again dying due of simple infections.

Alexander Fleming, discoverer of penicillin.
Types of antibiotic
Carbapenems
(meropenam, penicillin, cephalosporins)
Widely used and highly effective. Used for severe or high-risk infections including bacterial meningitis and septicaemia.
Fluoroquinolones
(ciprofloxin)
Widely used to treat common infections such as urinary tract infections and respiratory infections.
Aminoglycosides
(gentamicin)
Used in hospital for serious illness (septicaemia), with some serious side effects such as hearing loss and kidney damage.
Tetracyclines
(tigecycline)
Widely used against UTIs, sexually transmitted infections and even, unusually, some non-bacterial infections (such as Lyme’s disease).
How are antibiotics given?
Antibiotics can be taken orally (tablets or liquid medicine), applied as a cream or spray, or given via a drip or injection. These treatments must be taken as prescribed in order for them to work effectively. To reduce the risk of resistance arising, users should always follow the exact treatment guidance, even if they start to feel better quickly.
Antibiotics do not have any effect on viral or fungal infections such as cold, flu, most coughs and sore throats, athlete’s foot and thrush. Taking them for these conditions increases the risk of you and your family having longer or more severe illness.
We aim to educate people about the important role we all play in preventing this global health catastrophe, starting with taking antibiotics only as advised by doctors.

Side effects, interactions and allergies
Although serious side effects from taking antibiotics are rare, mild side effects such as nausea, sickness, bloating, indigestion and diarrhoea can be common. Some types of antibiotics can cause negative reactions when taken alongside other drugs, such as contraceptives or alcohol.
The human body is host to a range of bacteria that are beneficial, too, such as the various types found in the gut (the ‘gut microbiome’). Research has suggested that the balance of this microbiome is important for good health, and that taking antibiotics can disrupt this balance. Find out more about bacteria in the human body.
You should always read the instructions that come with antibiotics you are prescribed. Some may suggest measures to help prevent side effects, such as avoiding bright sunlight (due to photosensitivity) or not lying down immediately after taking the tablet (to prevent possible irritation of your oesophagus).
Some people are allergic to antibiotics, particularly penicillin and cephalosporins.
Why are there no new antibiotics?
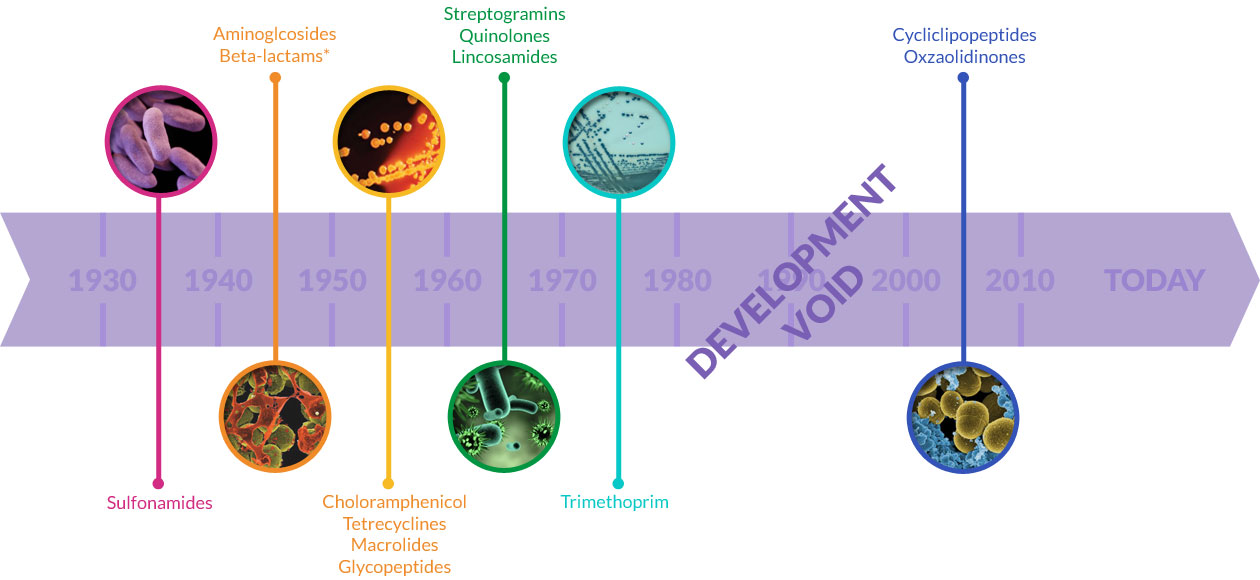
In the past 40 years we have only discovered two new types of antibiotic. It can cost billions of pounds and many years to create a new antibiotic, and bacteria can become resistant to a new treatment within a few years, or even months.
Fast developing resistance means that pharmaceutical companies may not have time to make back the money invested in creating the new drug before it falls out of use. This is particularly true as antibiotics are usually given for a short amount of time. Drugs for other conditions may be prescribed for years at a time, giving the companies more stable income.

Reserving any newly developed treatment for only those people with antibiotic-resistant infections would add to the problem. Pharmaceutical companies would have even fewer opportunities to derive income from the medicine.
Additionally, governments hold down the price of antibiotics, leaving little financial incentive for pharmaceutical companies to invest in research. The UK Government announced in January 2019 a new Five-Year AMR (antimicrobial resistance) Strategy (2019-2024) in which a new reimbursement scheme for antibiotics would be introduced based on their value to the NHS.
Funds for the scheme will be derived from the anticipated savings on reduced antibiotic prescribing, which is targeted to fall 15% by 2024. This would release just £30 million of new funding, based on the annual cost of antibiotics £200 million. Read our critique of the new strategy.
We’re committed to helping fund the development of new antibiotics and alternative therapies. But, we cannot work alone, we need your help to develop new antibiotic treatments.

